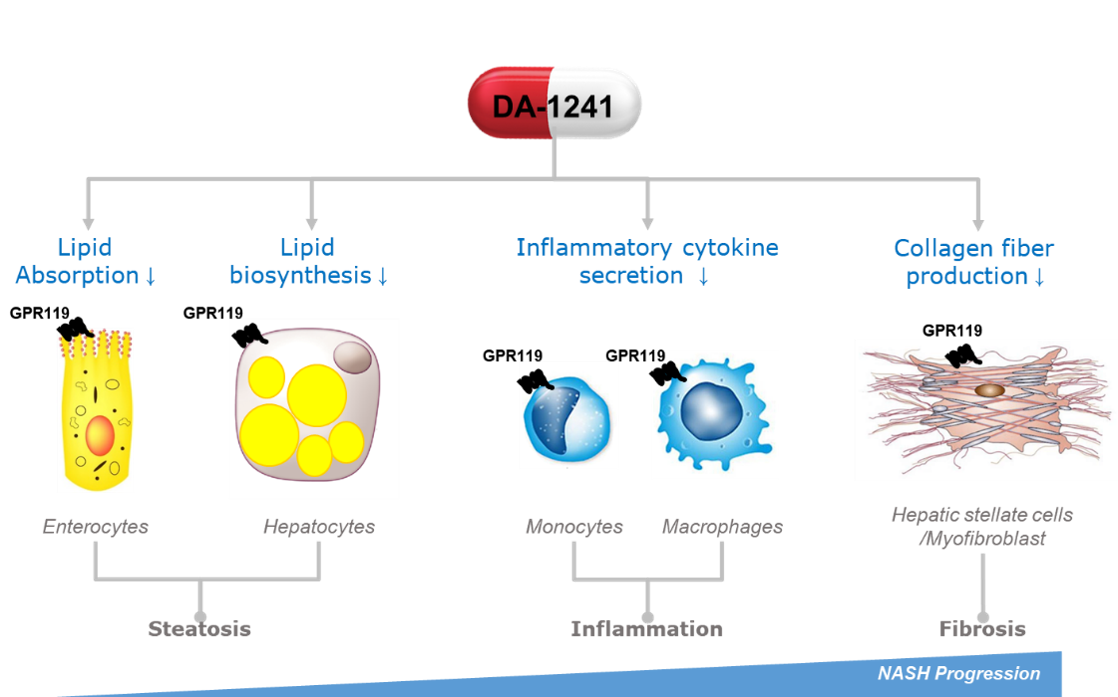
DA-1241 is a new chemical agent activating G protein-coupled receptor 119 (GPR119) mainly in the pancreas, intestine, and liver. In non-clinical studies, GPR119 activation by DA-1241 in hepatocytes, macrophages, and hepatic stellate cells inhibits lipid accumulation, immune cell infiltration, and the production of collagen fibers in the liver, directly ameliorating MASH pathophysiology such as steatosis, inflammation, and fibrosis. Moreover, GPR119 has a distinctive role in glucose and lipid metabolism via stimulating secretion of insulin and glucagon-like peptide-1 (GLP-1) in pancreatic beta cells and intestinal L-cells, respectively. Therefore, DA-1241 can also provide additional metabolic benefits in MASH patients with common comorbid metabolic diseases such as type 2 diabetes and dyslipidemia.
In Phase 1b clinical trials, the safety and efficacy of DA-1241 monotherapy were successfully confirmed. DA-1241 was well-tolerated in type 2 diabetic patients. GPR119 activation by DA-1241 treatment increased the plasma levels of gut peptide hormones (total GLP-1, PYY, GIP) as plasma concentrations of DA-1241 went up and showed a persistent and similar postprandial glucose-lowering activity to JANUVIA® (an oral anti-diabetic agent as a dipeptidyl peptidase inhibitor) in a head-to-head trial after 8 weeks of once daily oral treatment.
1. Comprehensive Review of Cardiovascular Disease Risk in Nonalcoholic Fatty Liver Disease. J Cardiovasc Dev Dis. 2022;9(12):419. PMID: 36547416, PMCID: PMC9786069, DOI: 10.3390/jcdd9120419
2. Hyperglycemia as a cardiovascular risk factor. Am J Med. 2003;115 Suppl 8A:6S-11S. PMID: 14678859 DOI: 10.1016/j.amjmed.2003.09.009; Fasting and Postchallenge Glycemia and Cardiovascular Disease Risk: The Framingham Offspring Study. Diabetes Care. 2002;25(10):1845-1850. PMID: 12351489 DOI: 10.2337/diacare.25.10.1845; Relationship between Hyperlipidemia, Cardiovascular Disease and Stroke: A Systematic Review. LDL subfractions are associated with incident cardiovascular disease in the Malmö Prevention Project Study. Atherosclerosis. 2017;263:287-292. PMID: 28728064 DOI: 10.1016/j.atherosclerosis.2017.07.003
